7. Gastroesophageal Reflux Disease – When Your Stomach Fights Back
The human body is a complex network of systems working together. When one system starts to malfunction, it can send signals that are felt in seemingly unrelated areas. One such example is gastroesophageal reflux disease (GERD), a digestive disorder that can cause chest pain mimicking that of a heart condition.
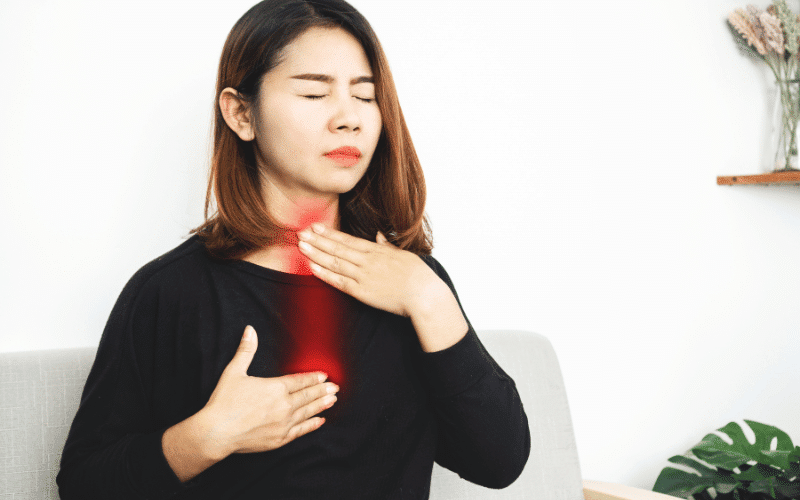
GERD occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach, causing irritation to the lining of the esophagus. This backward flow, or ‘acid reflux’, can result in a burning sensation in the middle of the chest, often after eating. This chest discomfort, commonly referred to as ‘heartburn’, can give a false alarm of a heart problem.
However, it’s not just heartburn that’s indicative of GERD. The condition can present other symptoms like a sour or bitter-tasting acid backing up into your throat or mouth, difficulty swallowing, the feeling of a lump in your throat, or chronic cough. Night-time symptoms or a worsening of symptoms when you’re lying down or bending over can also suggest GERD.
Why does GERD happen, you ask? The primary cause is the weakening or improper functioning of the lower esophageal sphincter (LES), a ring of muscle at the entrance of your stomach. Normally, the LES closes as soon as food passes through it. But if it doesn’t close all the way, or if it opens too often, acid produced in your stomach can move up into your esophagus, causing symptoms of GERD.
Factors that can increase your risk of GERD include obesity, pregnancy, hiatal hernia, smoking, asthma, diabetes, and delayed stomach emptying. Certain foods and drinks can also trigger or worsen GERD symptoms. These include fatty or fried foods, tomato sauce, alcohol, chocolate, mint, garlic, onion, and caffeine.
But fret not, if you’re diagnosed with GERD, there are several treatment options available. Depending on the severity of your symptoms, your doctor might recommend lifestyle changes, over-the-counter medications, prescription medications, or even surgery in some cases. Lifestyle changes can include avoiding foods that trigger your symptoms, eating smaller meals, not lying down after a meal, and maintaining a healthy weight.
Remember, though GERD is a common cause of chest pain, it’s crucial not to self-diagnose. Chest pain should never be dismissed. Always seek professional help to rule out other more serious causes, particularly heart-related problems.
Knowledge is power, and understanding the body’s complex systems and their signals can empower you to make informed health decisions. Whether it’s your stomach fighting back or a more severe condition, it’s crucial to listen to your body and respond appropriately. Your health is always worth fighting for. (7)