Introduction: The Silent Inflammatory Condition
In the vast spectrum of gastrointestinal disorders, microscopic colitis might seem like a minor blip. Yet, for those who suffer from it, the condition can be profoundly disruptive. What makes microscopic colitis particularly intriguing is its deceptive nature. Unlike many other digestive disorders, its symptoms aren’t easily visible, often leading to misdiagnosis or a lack of diagnosis entirely.
Though it may not garner as much attention as its more well-known counterparts like Crohn’s disease or ulcerative colitis, understanding microscopic colitis is crucial. This ailment affects a significant portion of the population, particularly those over the age of 50. As its name suggests, the signs of this condition are microscopic, and therefore, cannot be observed without specialized equipment. This aspect often leaves both patients and physicians perplexed and in search of answers.
Given its elusive nature, there’s a pressing need to shed light on microscopic colitis. In this article, we dive deep into 15 pivotal facts that illuminate the intricacies of this condition, offering insights into its causes, symptoms, treatment options, and more. By the end, you’ll possess a holistic understanding of microscopic colitis and the tools to navigate its challenges.
Fact 1: What Exactly is Microscopic Colitis?
The world of gastrointestinal disorders is vast and intricate, with each condition presenting its unique challenges. Microscopic colitis, often hidden in the shadows of its more prominent counterparts, emerges as an enigma in this domain. At its fundamental level, it’s an inflammation of the colon. Yet, what sets it apart is its microscopic nature. Traditional examinations won’t spotlight it, making it an elusive diagnosis.
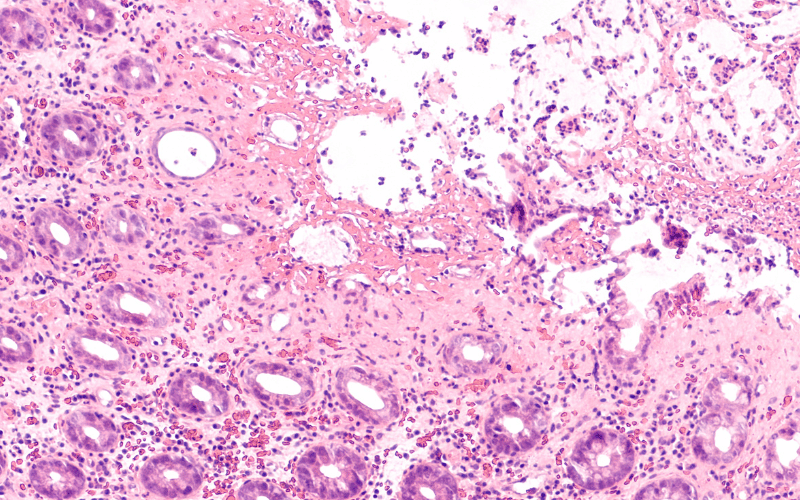
But why the term “microscopic”? The inflammation markers of this disorder, while significant in impact, are tiny in appearance. So tiny that they’re invisible during standard medical examinations and require specialized microscopic evaluation. This necessity often makes the initial discovery phase of the disease a bit cumbersome, leading to potential delays in diagnosis.
Diving deeper into its intricacies, we encounter two subtypes: collagenous colitis and lymphocytic colitis. While they share a similar symptom profile, the distinguishing factors lie in their microscopic appearance and underlying tissue changes. Collagenous colitis, for instance, sees a thickening of a protein layer in the bowel lining. Lymphocytic colitis, on the other hand, is marked by an increased presence of white blood cells in the bowel lining.
Awareness about this condition is pivotal. Despite its microscopic nature, its influence on a patient’s life can be macroscopic, affecting daily activities, comfort, and overall well-being. It’s not just about understanding the disease but also recognizing its silent yet profound impact on those who suffer from it.
Microscopic colitis, while small in name, is substantial in its implications. Comprehending its nature, challenges, and manifestations paves the way for better therapeutic interventions and more holistic patient care. (1)