Introduction: Navigating Through Chronic Pancreatitis
Embarking on the journey to understand chronic pancreatitis is essential for those impacted by this persistent condition.

The following segments will delve into a detailed exploration of 15 key facets of chronic pancreatitis, aiming to shed light on its intricate aspects. This endeavor seeks to empower patients, caregivers, and healthcare professionals with the knowledge and tools necessary for managing and navigating through the complexities of this condition.
Chronic pancreatitis, a condition marked by ongoing inflammation of the pancreas, necessitates a thorough understanding of its numerous dimensions. The pancreas, an indispensable organ situated behind the stomach, plays a crucial role in digesting food and regulating blood sugar. When chronic inflammation sets in, it hampers the organ’s ability to carry out these vital functions, leading to a variety of symptoms and potential complications.
When delving into the causes of chronic pancreatitis, it’s apparent that the condition stems from a multitude of sources. Prevalent causes include excessive alcohol consumption and gallstone formation.
Nonetheless, genetic factors, autoimmune responses, and recurrent bouts of acute pancreatitis also contribute significantly to the condition’s onset. Recognizing and addressing these root causes is imperative for effective management and mitigation of the condition’s impact.
The symptomatology of chronic pancreatitis is diverse, with individuals commonly experiencing abdominal pain, nausea, vomiting, unintended weight loss, and steatorrhea (oily stools). The abdominal pain associated with the condition can be particularly intense and life-disrupting, necessitating prompt and accurate diagnosis.
Navigating through the diagnostic process of chronic pancreatitis requires a multifaceted approach. Healthcare professionals typically rely on a combination of clinical evaluations, advanced imaging techniques like CT scans and MRIs, endoscopic ultrasounds, and various laboratory tests. This thorough investigative process is vital for distinguishing chronic pancreatitis from other potential causes of similar symptoms, ensuring that patients receive the most appropriate and effective care.
With a clear understanding of the condition, its causes, symptoms, and diagnostic approaches, we are now poised to delve deeper into the 15 crucial facts about chronic pancreatitis. These facts will provide a more nuanced view of the condition, enhancing our collective understanding and ability to effectively manage it.
1. Chronic Pancreatitis: An Overview
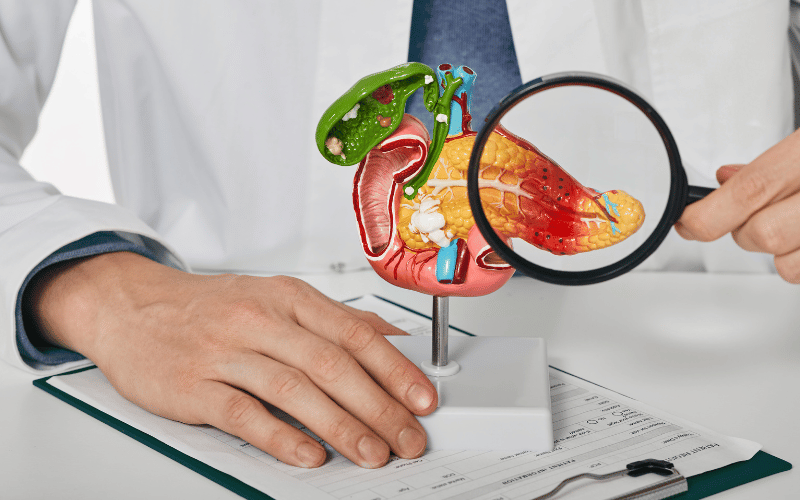
Chronic pancreatitis is a lasting inflammation of the pancreas. This is the organ responsible for producing enzymes and hormones that help break down foods and regulate blood sugar.
In chronic pancreatitis, the inflammation damages the organ’s tissue. This damage affects its ability to function properly.
The lasting damage can cause scar tissue to form. This scar tissue can block the flow of digestive enzymes.
When these enzymes get trapped, they can start to digest the pancreas itself. This process leads to pain and further damage.
Over time, the pancreas can lose its ability to produce enough enzymes and hormones. This deficiency can lead to digestive problems and diabetes.
The condition is most common in people between 30 and 40 years of age. But, it can affect anyone. It tends to be more common in men than women.
People with a history of alcohol abuse or gallbladder disease are at higher risk. Other risk factors include smoking, a family history of pancreatitis, and certain genetic mutations.
It’s crucial to diagnose and manage chronic pancreatitis early. This can help prevent further damage to the pancreas.
It can also help manage symptoms and improve quality of life. The management often includes lifestyle changes, medications, and sometimes surgery. Regular follow-up care with a healthcare provider is essential. (1)