Cause 3: Multiple Blood Transfusions
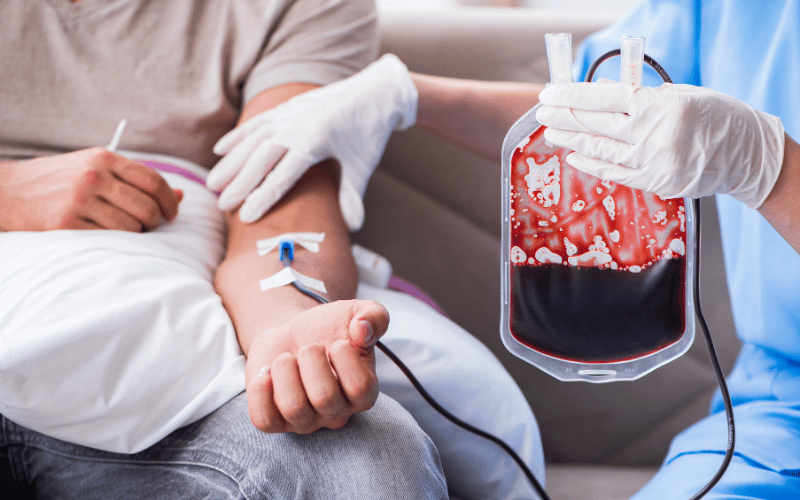
Individuals requiring frequent blood transfusions, such as those with certain types of anemia or chronic blood disorders, face an increased risk of hemochromatosis. Each transfusion introduces additional iron into the body. Over time, and without proper management, this iron can accumulate to dangerous levels, primarily in the liver, heart, and endocrine glands, leading to iron overload and its associated complications.
Blood transfusions are life-saving and often necessary, but they come with the responsibility of regular monitoring and management of iron levels. It’s crucial for healthcare providers and patients to be vigilant, keeping a close eye on iron levels and taking preemptive actions to prevent iron overload.
Therapeutic phlebotomy, a procedure to remove blood from the body, becomes a vital tool in such cases. By regularly drawing blood, similar to a blood donation, excess iron is removed from the body, helping maintain balanced iron levels and preventing hemochromatosis.
Dietary management also plays a role, with patients being advised to avoid excessive iron and vitamin C intake, as vitamin C enhances iron absorption. A balanced diet, along with regular medical check-ups, ensures that the benefits of blood transfusions are not negated by the risk of iron overload.
Closing this point, while multiple blood transfusions pose a risk for hemochromatosis, through careful monitoring, therapeutic interventions, and informed dietary choices, individuals can effectively manage their iron levels, preventing iron overload and safeguarding their health. (3)