Introduction: A Closer Look On The Family of Inflammatory Bowel Diseases
Inflammatory Bowel Disease (IBD) is a term that encompasses a group of disorders characterized by chronic inflammation of the gastrointestinal tract. The most prominent players in this group are Ulcerative Colitis (UC) and Crohn’s Disease (CD). These conditions, while sharing commonalities, each have their distinct clinical presentations, complications, and management strategies, affecting patients’ quality of life in unique ways.
The prevalence of UC and CD has been steadily increasing over the past few decades, impacting millions of individuals worldwide. They present with a spectrum of symptoms ranging from abdominal pain, diarrhea, weight loss, to systemic manifestations such as fatigue. This complex symptomatology often leads to delayed diagnosis, primarily due to the overlap between the symptoms of the two diseases.
However, UC and CD are not merely two faces of the same coin. They each carry a distinct clinical identity, with unique characteristics that set them apart. Accurately distinguishing between the two is not merely an academic pursuit; it holds immense implications for the management and prognosis of the patient. The location and depth of the disease, risk of complications, and response to treatment all vary between UC and CD, necessitating a precise diagnosis.
The path to distinguishing UC from CD is paved with an understanding of their key differences. By dissecting these differences, we aim to provide clarity that can guide patients, their caregivers, and healthcare providers on their journey through these perplexing diseases. In this article, we will delve into six distinguishing features: anatomical location, depth of inflammation, endoscopic appearance, complications, cancer risk, and treatment response.
While Ulcerative Colitis and Crohn’s Disease share a common umbrella of Inflammatory Bowel Disease and have overlapping symptoms, they are distinct entities with unique characteristics. As we unravel these six key differences, we hope to empower you with knowledge and understanding, allowing for informed decision-making, and more nuanced management of these complex conditions.
Difference 1: Anatomical Location – The Battlefield of Disease
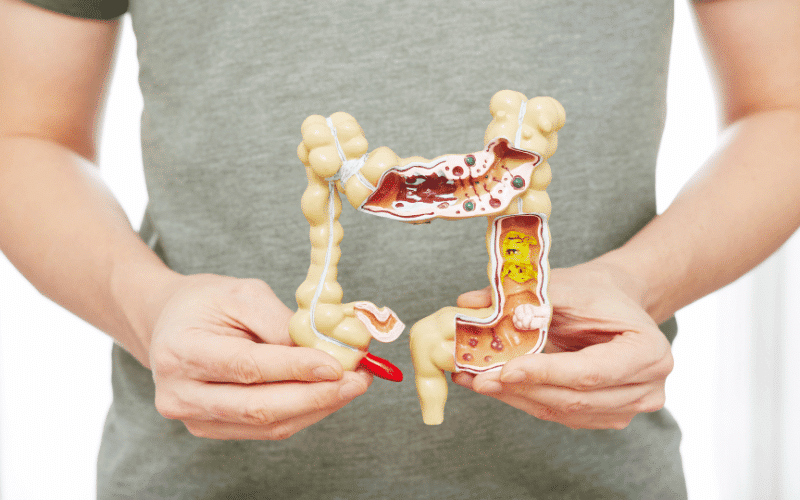
The first distinguishing feature between UC and CD is the location within the gastrointestinal tract where the disease manifests. In UC, the disease is confined to the colon or large intestine, beginning in the rectum and extending upwards in a continuous manner. This implies that in UC, the disease starts from the rectum and spreads upward towards the colon, but never beyond.
Conversely, CD can manifest anywhere along the digestive tract, from the mouth to the anus, although it most commonly affects the terminal ileum or the end of the small intestine. Unlike UC, CD doesn’t follow a predictable path. Its presence can be scattered throughout different sections of the digestive tract, leading to a patchy distribution, often referred to as “skip lesions.”
The implications of these differences in anatomical locations are significant. They influence the presenting symptoms, disease progression, and the approach to treatment. For instance, patients with CD often present with symptoms associated with small intestinal disease, such as nutrient malabsorption, while UC is typically associated with symptoms of colonic disease, like bloody diarrhea.
Furthermore, the unpredictability of CD’s location can pose challenges in diagnosis and treatment. CD’s propensity to affect any part of the digestive tract means it can lead to symptoms that might not be immediately associated with a bowel disorder, such as oral ulcers if the disease affects the mouth. This can lead to delays in diagnosis and treatment. (1)