Introduction: Setting the Context on Hepatocellular Carcinoma (HCC) Prognosis
Hepatocellular carcinoma (HCC) stands as the dominant form of primary liver cancer, asserting its presence prominently in medical research and health discussions worldwide. For many patients grappling with an HCC diagnosis, prognosis – or the future course and likely outcome of the disease – remains a paramount concern. Yet, the terrain of HCC prognosis is layered, influenced by myriad factors ranging from early detection to the nuances of treatment modalities.
Diving into the heart of HCC prognosis is akin to navigating a labyrinth. Each turn and corridor represents a different variable that can shape the outlook for a patient. Consider the role of cirrhosis, for instance. A liver laden with scars from cirrhosis is not just a testament to its battle with long-term damage, often from conditions like hepatitis or alcoholism, but also a beacon signaling the likelihood of a challenging prognosis.
Beyond cirrhosis, the landscape gets even more intricate. Tumor size, vascular invasions, underlying liver functions, and even blood markers like Alpha-fetoprotein (AFP) levels – each of these plays a part in the story of HCC prognosis. However, while these elements might seem overwhelming, understanding them individually and collectively is pivotal. Not only does this comprehension empower patients and caregivers with knowledge, but it also illuminates the path forward, guiding treatment decisions and managing expectations.
In the subsequent sections, we will meticulously explore each facet of HCC prognosis. Ten crucial insights await, poised to offer clarity and depth to this critical subject. As we navigate through each, remember: while HCC’s prognosis can be challenging, knowledge is empowering. Let’s embark on this enlightening journey together.
Fact 1: The Power of Early Detection
Early detection in any cancer is a game-changer, and Hepatocellular carcinoma (HCC) is no exception. Recognizing HCC in its beginning stages can dramatically alter the trajectory of the disease. In these early stages, the cancer is likely confined to the liver. This confinement offers a greater range of effective treatment options, from surgeries to targeted therapies.
As the tumor remains localized, interventions can be more precise, and the chances of a successful treatment increase manifold. Furthermore, early detection reduces the potential of metastasis. Metastasis, or the spread of cancer cells to other parts of the body, often complicates treatment strategies and prognosis.
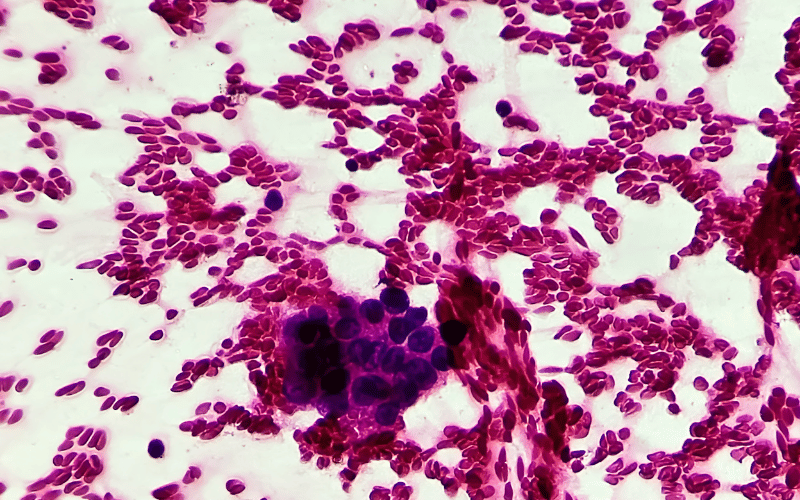
The tools for early detection, such as regular liver function tests, imaging, and biopsies, are now more accessible than ever. Advancements in medical imaging have provided clearer views of the liver, making it possible to spot even small anomalies. Furthermore, understanding the importance of early detection encourages at-risk populations, such as those with a history of liver disease, to opt for regular screenings. (1)