Symptom 9: Relative Afferent Pupillary Defect (RAPD) – The Eye’s Telltale Signal in Optic Neuropathy
In the landscape of optic neuropathy symptoms, one marker that speaks volumes is the relative afferent pupillary defect or RAPD. It’s a mouthful, indeed, but its significance in diagnosing optic neuropathy is unquestionable.
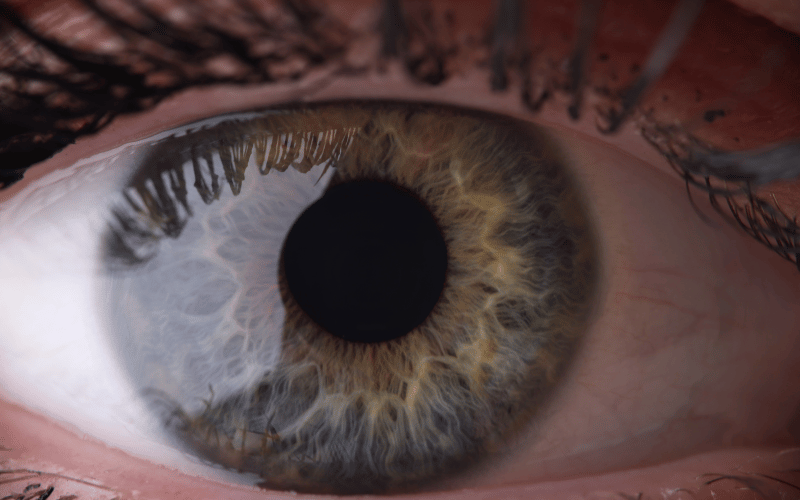
So, what’s the tale that our pupils are trying to tell us? The story unfolds when a light is shone into one eye, causing both eyes to constrict. This natural reaction, known as the pupillary light reflex, keeps the amount of light entering the eyes in check. However, with RAPD, the affected eye’s reaction to light becomes abnormal, giving off a critical clue to underlying optic nerve issues.
This oddity occurs due to the damaged optic nerve’s inability to properly transmit the information about light levels. The brain doesn’t receive the correct signals and, as a result, fails to control the pupil’s constriction effectively. An observer can notice this defect when a swinging flashlight test is conducted, revealing the affected eye’s lesser response to light compared to the healthy one.
While it might seem like an odd symptom to the layperson, RAPD is a well-recognized and significant marker for optic neuropathy within the medical community. Its detection plays a critical role in diagnosing optic neuropathy, particularly in cases where the disease’s more visible symptoms are not yet apparent.
In the end, RAPD is a great example of how our bodies are full of subtle but crucial clues that speak volumes about our health. It underlines the fact that the presence of optic neuropathy may sometimes be hidden in the eyes’ response to light, emphasizing the need for comprehensive eye exams in early disease detection and management. (9)