Introduction: The Vital Importance of Understanding RMS Prognosis
When the term Rhabdomyosarcoma (RMS) is mentioned, a whirlwind of questions arises, often centered around prognosis and what the future may hold. As one of the most predominant soft tissue tumors affecting children and adolescents, RMS remains a focal point in the realm of oncological research. Knowledge of its prognosis not only illuminates the journey ahead but also empowers patients and their loved ones to make informed decisions.
Although RMS is relatively rare, it’s impact, both emotionally and physically, on patients and their families is profound. A prognosis, in essence, provides a forecast, a glimpse into the probable course and outcome of the disease. For anyone embarking on the RMS journey, understanding this forecast can be an invaluable tool, a beacon of light in times of uncertainty.
But why is there such a pressing need to understand the prognosis of RMS? The answer lies in its complexity and variability. Different subtypes of RMS, locations of the tumor, and other critical factors can significantly influence the projected outcome. A singular prognosis doesn’t fit all, emphasizing the necessity to delve deep, gather facts, and tailor the understanding to each unique case.
In the coming sections, we aim to distill the most pertinent facts about RMS prognosis. This will not just be a compilation of statistics, but a comprehensive exploration into what those numbers signify, how they intertwine with individual stories, and the hope and advancements they herald for the future.
Our mission is to bring clarity, reduce the overwhelming nature of medical jargon, and offer a solid foundation upon which patients, caregivers, and medical professionals can stand, united in their journey against Rhabdomyosarcoma.
1. What is Rhabdomyosarcoma (RMS)?: A Glimpse into the Disease’s Nature
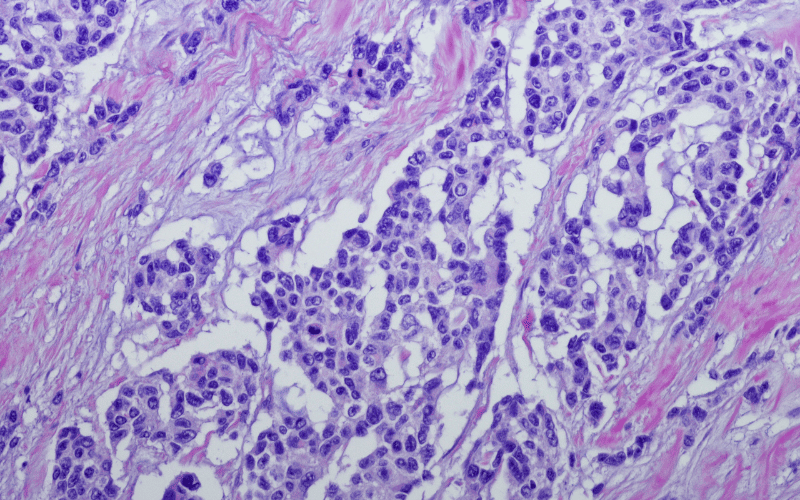
Rhabdomyosarcoma is a term that often evokes questions and curiosity. At its core, it is one of the most dominant soft tissue tumors affecting the younger generation. Its origin, mainly from skeletal muscle progenitor cells, sets it apart from other cancers.
Diving deeper, RMS can be categorized into several subtypes. Each subtype behaves differently, presents its unique challenges, and demands specialized treatment protocols. While the embryonal type is more prevalent among younger children, the alveolar subtype is relatively aggressive and often diagnosed in older kids.
The alarming part of RMS is its ability to occur anywhere in the body. Common sites include the head, neck, bladder, and reproductive organs. Yet, it can be elusive, appearing in places one wouldn’t typically suspect. This versatility is one of RMS’s hallmarks, making its prognosis and treatment a challenge. (1)