Consequence 9: Possibility of Fetal Growth Restriction
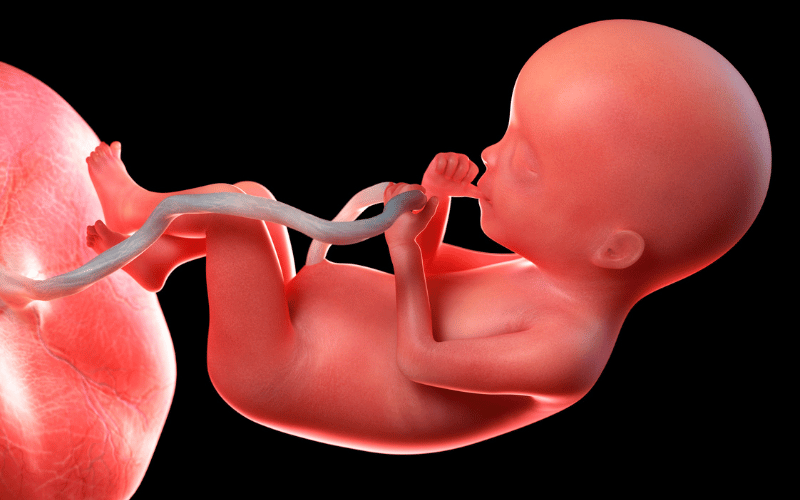
Contrary to the risk of fetal macrosomia, diabetes can also result in fetal growth restriction (FGR), particularly when vascular complications impair placental blood flow. FGR is a condition where a fetus is unable to achieve its genetically predetermined size, often leading to a range of complications.
High-risk obstetricians monitor fetal growth closely in pregnancies complicated by diabetes, employing ultrasound measurements to track fetal size and amniotic fluid levels. The placental function is assessed, and doppler flow studies may be conducted to evaluate blood flow to the fetus.
Nutritional support is tailored to support optimal fetal growth, with emphasis on managing blood glucose levels to ensure a steady supply of nutrients to the fetus. Blood sugar fluctuations can impact the placenta’s ability to nourish the fetus, making consistent glycemic control imperative.
When FGR is diagnosed, the timing of delivery becomes a critical decision. While prolonged in-utero growth is beneficial, it must be balanced against the potential risks of continued exposure to a suboptimal environment. This may lead to considerations of early delivery, depending on the severity of growth restriction and overall fetal well-being.
Despite these challenges, with proactive surveillance and management, most women with diabetes can successfully navigate the risks of FGR, delivering healthy infants who thrive postnatally with appropriate neonatal care. (9)