2. Multiple System Atrophy (MSA): The Insidious Multi-Front Battle
As we venture further into the realm of ataxia, another critical player emerges from the shadows—Multiple System Atrophy (MSA). This progressive neurodegenerative disorder is second on our list and serves as a vivid example of the complex ways in which ataxia can manifest.
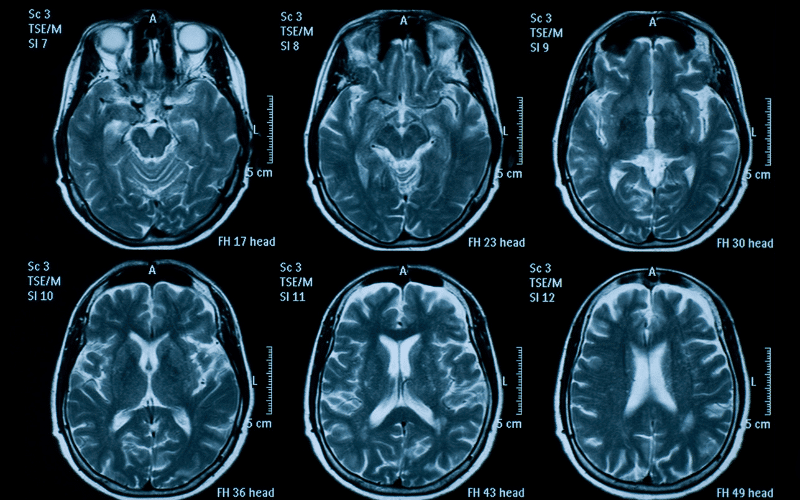
MSA is aptly named, encapsulating the essence of this condition—multiple systems within the body deteriorate over time due to a gradual loss of function in specific areas of the brain, including the basal ganglia, cerebellum, and brainstem. These regions play a vital role in regulating motor functions, balance, and other automatic functions like blood pressure control. When these systems falter, a cascade of symptoms ensues, including the characteristic loss of coordination seen in ataxia.
But what triggers MSA? The exact cause remains a mystery, but scientists have linked this condition to the accumulation of a protein called alpha-synuclein in brain cells. These protein deposits disrupt normal cell functions and eventually lead to cell death.
The onset of MSA typically occurs in adulthood, often striking in the 50s or 60s. It’s a tricky condition to diagnose, given the broad spectrum of symptoms, many of which overlap with other disorders.
In the early stages, patients might experience postural hypotension, a condition where their blood pressure drops significantly upon standing, leading to dizziness or fainting. This autonomic dysfunction is often the first clue pointing towards MSA. As the disease progresses, other signs like ataxia, rigid muscles, slow movements, and speech difficulties start to surface. (2)