Frequently Asked Questions (FAQs) about Basal-Cell Carcinoma
Advertisements
 Advertisements
Advertisements
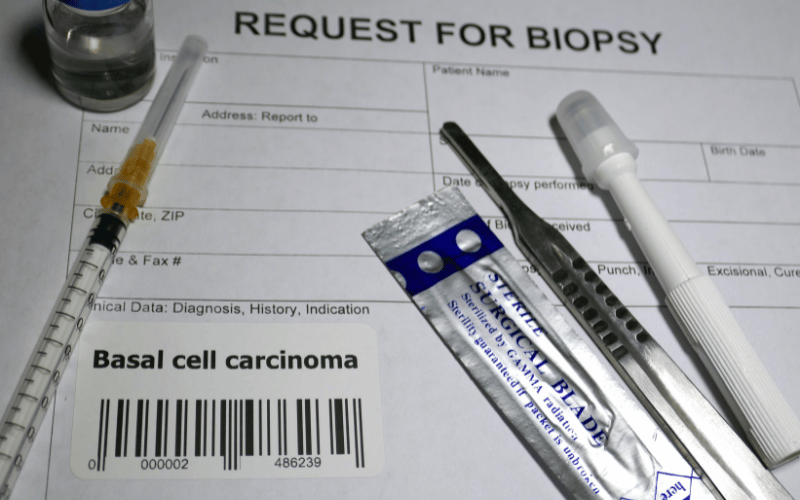
1. What is basal-cell carcinoma (BCC)?
Basal-cell carcinoma, commonly referred to as BCC, is the most prevalent type of skin cancer. It originates from the basal cells, which are situated in the epidermis (the skin’s outermost layer). Unlike other forms of skin cancer, BCC tends to grow slowly and is primarily localized, meaning it is less likely to spread to other parts of the body.
2. What causes BCC?
Prolonged exposure to ultraviolet (UV) radiation is the leading cause of BCC. This exposure can come from the sun or from artificial sources like tanning beds. Other factors, such as having light-colored skin, a family history of BCC, or exposure to certain chemicals, can also increase the risk.
3. How can I differentiate BCC from other skin issues?
BCC has distinct symptoms like open sores that don’t heal, red patches, shiny bumps, and scar-like areas. However, diagnosing BCC just based on appearance can be challenging since many of its symptoms overlap with other skin conditions. If you’re suspicious of any skin changes or lesions, it’s crucial to see a dermatologist for a professional evaluation.
4. How is BCC treated?
Treatment options for BCC depend on its type, size, location, and depth of penetration, as well as the patient’s age and overall health. Common treatments include surgical removal, Mohs surgery (a procedure to remove the tumor layer by layer), freezing (cryosurgery), topical treatments, radiation therapy, and laser surgery.
5. Is BCC fatal?
BCC itself is not typically life-threatening. However, if left untreated, it can cause significant disfigurement or damage to the skin and underlying tissues. It’s essential to detect and treat BCC early to prevent complications and potential spreading, although it rarely metastasizes or spreads to other parts of the body.
6. How can I prevent BCC?
The best prevention is to protect your skin from the sun. Avoid direct sunlight during peak UV hours (usually between 10 a.m. and 4 p.m.), wear protective clothing, use a broad-spectrum sunscreen with at least SPF 30, and avoid tanning beds. Regular skin self-exams and professional skin examinations can also help in early detection.
7. I had BCC once. Can it come back?
Yes, if you’ve had BCC once, you’re at a higher risk of developing a new BCC in the future. Regular follow-ups with a dermatologist and self-skin examinations are crucial to monitor any new or returning growths.
Conclusion: Understanding and Addressing Basal-Cell Carcinoma
In the vast spectrum of skin conditions, basal-cell carcinoma (BCC) stands out not only for its prevalence but also for its deceptive subtlety. As the most common type of skin cancer, BCC presents itself through varied symptoms—ranging from innocuous shiny bumps to more alarming non-healing sores. However, its slow-growing nature means it often goes unnoticed until it becomes more pronounced.
Thankfully, the medical community is well-equipped to handle BCC, offering an array of treatments tailored to the severity and location of the carcinoma. But prevention remains our most potent weapon.
The role of UV exposure in the development of BCC can’t be emphasized enough. As we forge ahead, equipped with the knowledge of its symptoms and causes, let’s pledge to be more proactive. Whether it’s opting for SPF-rich sunscreens, protective clothing, or regular skin check-ups, these steps, though simple, can be the barrier that stands between us and the potential risks of BCC.
Finally, it’s essential to remember that our skin tells stories—of our adventures, our encounters, and sometimes, our health. By being vigilant observers, we can ensure that the tales it narrates are ones of health, care, and well-being.