Introduction: Navigating the Landscape of Impaired Fasting Glucose
Impaired Fasting Glucose (IFG), a state often preceding the onset of type 2 diabetes, is a health concern that has been increasingly prevalent in today’s fast-paced lifestyle. Characterized by higher than normal blood sugar levels after an overnight fast, IFG serves as a crucial indicator, pointing towards the body’s dwindling efficiency in managing blood glucose levels. The significance of understanding and identifying IFG lies in its subtlety – the condition often manifests without conspicuous symptoms, making awareness and knowledge about it all the more vital.

The journey of recognizing IFG begins with an understanding of what it entails. In simple terms, IFG is a metabolic state where the body begins to show resistance to insulin – a hormone responsible for regulating blood sugar levels. This resistance leads to a gradual and often unnoticed increase in fasting blood sugar levels. It’s a critical phase where intervention can significantly alter the course towards diabetes or revert back to normal glucose tolerance.
Understanding IFG also involves recognizing its risk factors. These include obesity, particularly abdominal obesity, a sedentary lifestyle, a family history of diabetes, and certain ethnic predispositions. The condition is more prevalent in adults, but with changing lifestyle patterns, it is increasingly being observed in younger populations as well. The importance of early detection of IFG cannot be overstated. It’s a condition that serves as a red flag, a warning sign that the body’s metabolism is not functioning optimally. Early detection opens the door to effective management strategies, including lifestyle modifications and, in some cases, medication. These interventions are crucial in preventing the progression of IFG to type 2 diabetes, a condition that carries with it an array of complications.
Moreover, understanding IFG extends beyond the realms of physical health. It has psychological and social dimensions as well. The diagnosis of IFG can be a wake-up call, prompting individuals to adopt healthier lifestyle choices. It also plays a significant role in healthcare planning and resource allocation, given the rising prevalence of diabetes globally. This article delves into the world of IFG, exploring its symptoms, risks, and management strategies. It’s designed to provide a comprehensive overview, aiding in the recognition of this silent health challenge and empowering individuals with the knowledge to act and prevent its progression.
Symptom 1: Slightly Elevated Blood Sugar Levels
Slightly elevated blood sugar levels are a pivotal indicator of Impaired Fasting Glucose (IFG). This state is characterized by fasting blood glucose levels that are higher than normal but not yet high enough to be classified as diabetes. These levels generally range between 100 to 125 mg/dL. It’s essential to comprehend that even a minor elevation can signify the onset of metabolic irregularities.
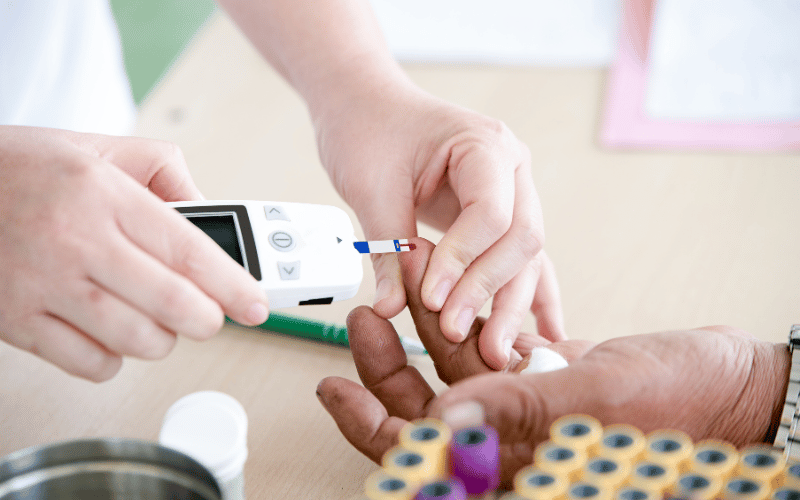
Regular monitoring of these levels is critical for individuals at risk. This includes people with a family history of diabetes, those who lead a sedentary lifestyle, or individuals who are overweight. Regular blood tests can help in early detection, thereby allowing for timely interventions.
Persistently elevated blood sugar levels, even if only slightly, can have long-term effects on one’s health. Over time, they can lead to the hardening of blood vessels, increasing the risk of cardiovascular diseases. It’s a gradual process that, if unchecked, can lead to serious complications.
Making lifestyle adjustments is key in managing these elevated levels. This includes adopting a diet low in refined sugars and carbohydrates, increasing physical activity, and maintaining a healthy weight. Such changes can significantly lower blood sugar levels, often bringing them back to normal.
In some cases, medical intervention may be necessary. Healthcare professionals might prescribe medication to help regulate blood sugar levels, especially if lifestyle changes alone are insufficient. It’s a collaborative approach, where both the individual and healthcare provider work together to manage the condition. (1)