Introduction: Plasma Cell Myeloma Unraveled
Plasma cell myeloma, more commonly known as multiple myeloma, stands as one of the most complex diseases of the blood. At its core, it’s a cancer that attacks plasma cells – a type of white blood cell responsible for producing antibodies. These malignant plasma cells accumulate in the bone marrow, overpowering healthy cells and leading to the production of abnormal proteins rather than useful antibodies.
Multiple myeloma remains an enigma for many. The disease doesn’t present itself through a singular symptom but rather a range of manifestations, making its early detection a challenge for even the most seasoned medical professionals. Its progression is marked by stages, each telling a unique story about the severity and spread of the disease. Understanding these stages is paramount not just for those diagnosed with the illness, but for caregivers and medical professionals aiming to provide the best care.
These stages aren’t mere numbers; they represent a spectrum, showcasing how the disease morphs and escalates. Recognizing the symptoms associated with each stage ensures timely interventions, ultimately aiding in better outcomes for patients. In the forthcoming sections, we’ll delve into each of these stages, shedding light on their intricacies and guiding you through the tumultuous journey of multiple myeloma.
Stage 1. Multiple Myeloma: A Subtle Onset
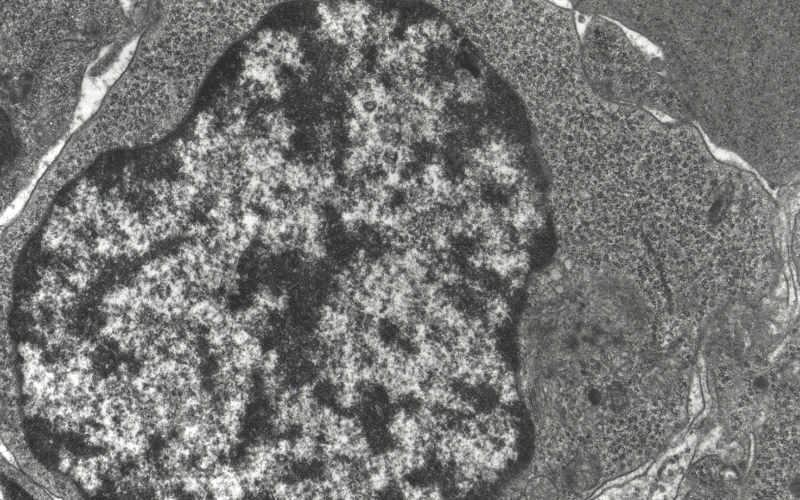
Stage I of multiple myeloma is like the quiet before the storm, where only faint ripples hint at what lies ahead. During this phase, the disease subtly plants its seeds, gradually making its way into the host’s system. Most patients in this stage remain oblivious to its existence. It sneaks in, affecting the bone marrow, causing it to produce an excess of abnormal plasma cells, which later form a specific type of protein that can be detrimental to kidney functions. At this nascent stage, the proliferation of these cells is limited, thus symptoms, if any, are barely noticeable.
A slight spike in the levels of this protein might be the only potential sign of the disease’s inception. Regular health screenings become the unsung heroes at this juncture. Through routine blood tests, one can detect the heightened protein level, specifically the monoclonal protein or M-protein. The kidneys, in their prime function, attempt to filter out this excess protein, but over time, with increasing levels, they might get overwhelmed, leading to complications down the line. This is why early detection can be crucial.
Another tool in detecting this sly disease is radiography. Even though there might not be apparent symptoms felt by the patient, an X-ray might show slight changes in bone structure. This doesn’t necessarily translate to full-blown bone lesions but can indicate slight alterations in bone density. These minuscule changes, often overshadowed by other more prominent health issues, might very well be the red flags that help in early diagnosis and subsequent management.
Physiologically, the patient might feel absolutely fine, dismissing any minor fatigue or occasional weakness as mere by-products of a busy life. Some might experience a vague sense of unwellness, but nothing pinpointed or pronounced. The human body, in its magnificent design, often adapts and compensates for minor malfunctions, masking potential problems. Hence, these soft whispers of symptoms might just go unnoticed unless one is exceptionally vigilant.
The silver lining of a Stage I diagnosis is the potential for a favorable prognosis. The disease, being in its infancy, has not wreaked havoc yet, giving medical professionals a chance to intervene early. With the right course of action, many individuals can continue leading a near-normal life, with periodic medical checks becoming a part of their routine. However, vigilance is crucial because, as benign as it might seem now, the tide can turn, making proactive health management paramount. (1)