Introduction: Tracheomalacia – An Insightful Overview
Tracheomalacia, a term that might sound complex at first, refers to a condition where the trachea (windpipe) is softer than usual. This softening can lead to a series of health challenges, particularly in breathing. While tracheomalacia might not be a household name, its impact on those affected is significant. This article aims to demystify tracheomalacia, offering crucial insights to anyone seeking to understand this condition better.

The trachea is our body’s airway conduit, a vital component of our respiratory system. In tracheomalacia, the tracheal walls weaken, potentially collapsing during breathing, especially when exhaling. This collapse can cause obstruction in the airflow, leading to a range of symptoms that are often alarming yet misinterpreted. Understanding these symptoms is key to early detection and effective management of the condition.
Who is most likely to be affected by tracheomalacia? This condition can be present at birth (congenital) or develop later in life (acquired). Congenital tracheomalacia is often discovered in infancy, while the acquired form usually manifests in adults. The reasons behind the development of tracheomalacia vary, ranging from developmental issues to external factors impacting the trachea over time.
Recognizing the symptoms of tracheomalacia is crucial for timely intervention. The most common sign is a high-pitched breathing sound, known as stridor, especially when the individual is lying down. However, it’s important to note that these symptoms can be confused with other respiratory conditions, underlining the importance of accurate diagnosis and specialized care.
With this introduction to tracheomalacia, we set the stage for a deeper exploration into its causes, symptoms, diagnosis, and management. Stay tuned as we delve into each aspect, equipping you with the knowledge to understand, identify, and address this condition effectively.
1. The Anatomy of Tracheomalacia: Understanding the Tracheal Structure
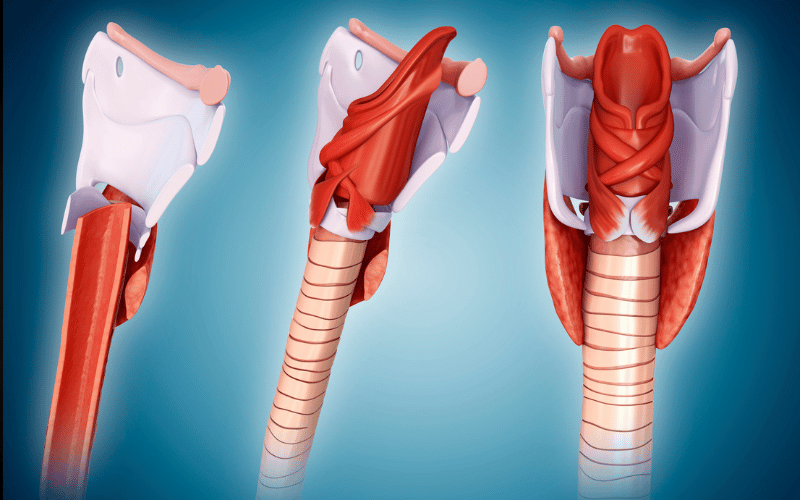
Tracheomalacia is deeply rooted in the structural aspects of the trachea. The trachea, commonly known as the windpipe, is a tube composed of rings of cartilage and muscle that keep it rigid. In tracheomalacia, these cartilaginous rings are weaker or less rigid, leading to the trachea’s collapse during breathing.
The collapse of the trachea during exhalation is a key feature of tracheomalacia. This phenomenon occurs because the weakened tracheal walls cannot withstand the normal pressures of breathing. As a result, the trachea narrows or flattens, which can significantly obstruct airflow.
Understanding this structural weakness is crucial in grasping how tracheomalacia affects the respiratory system. The condition can vary in severity – from mild, where individuals experience few symptoms, to severe cases that require immediate medical intervention. The degree of tracheal collapse often determines the severity of symptoms and the approach to treatment.
Exploring the variations in tracheal anatomy among individuals with tracheomalacia reveals intriguing patterns. Some may have a uniformly soft trachea, while others might have localized weak spots. These variations in structure play a vital role in the symptoms experienced and the management strategies employed.
This foundational knowledge of tracheal anatomy in tracheomalacia sets the stage for understanding its causes, symptoms, and potential treatments. As we explore further, the complexities of this condition unfold, highlighting the importance of individualized care and management strategies. (1)