Fact 11. The Diagnostic Challenge: Unraveling the Mystery of ALS
Diagnosing ALS is a complex process, often requiring several months of testing and observation. There’s no definitive test for ALS, making it a diagnosis of exclusion—meaning doctors must rule out other conditions before arriving at a diagnosis of ALS.
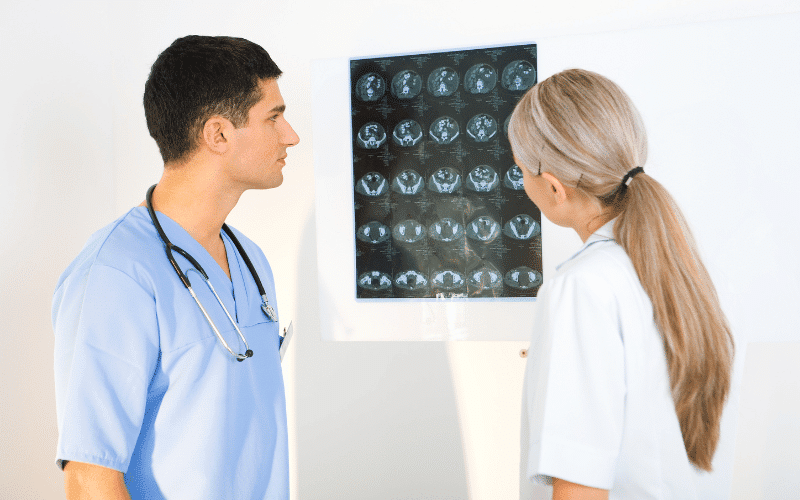
Initial symptoms can mimic a variety of neurological disorders, including multiple sclerosis, Parkinson’s disease, and peripheral neuropathy. This vast array of potential diagnoses necessitates a thorough evaluation, which may include blood tests, MRIs, and electrophysiological studies like electromyography (EMG) and nerve conduction studies (NCS).
An EMG involves inserting small needles into the muscle to record electrical activity, while NCS measures the speed and strength of signals traveling between the nerves and muscles. These tests can detect the characteristic pattern of nerve damage seen in ALS, providing crucial evidence to support the diagnosis.
The diagnostic process also includes a thorough clinical assessment. Neurologists look for signs of muscle weakness, atrophy, and fasciculations (small involuntary muscle twitches), as well as changes in reflexes. This clinical picture, in conjunction with the results from diagnostic tests, forms the basis of an ALS diagnosis. (11)