Introduction: A Deep Dive into the World of Esophageal Achalasia
Esophageal achalasia isn’t exactly a condition that’s the talk of the town. However, if you’re one of the unlucky ones battling it, you know all too well how life-altering it can be. Are you finding it difficult to swallow? Experiencing frequent regurgitation that’s not quite acid reflux? You might be dealing with the stubborn nemesis known as esophageal achalasia. Before diving into its peculiar symptoms, it’s critical to underline the importance of understanding this condition. Simply put, your quality of life is at stake.
Now, you might ask, “Why should I care?” Well, consider this: Esophageal achalasia is not just a one-off event; it’s a prolonged condition. It can mess with your day-to-day life, affecting everything from your diet to your emotional well-being. It can be as misleading as it is debilitating, often masquerading as more common gastrointestinal issues like heartburn or acid reflux. You need to be aware, not just for yourself but also to safeguard your loved ones, who may not even know what they’re dealing with.
You’re not alone in this; a growing number of people are searching phrases like, “Why can’t I swallow my food?” or “Unexplained chest pain during meals.” The symptoms range from annoying to alarming, and unfortunately, esophageal achalasia is often diagnosed late due to its misleading signs.
What’s coming up is a deep dive into the top 10 symptoms that signal the presence of this condition. We’re not just scratching the surface here; we’re digging deep, so you get the most precise, actionable information possible. And hey, this isn’t just a run-of-the-mill medical write-up. It’s your go-to source to understanding those nagging symptoms that have you running web searches at odd hours.
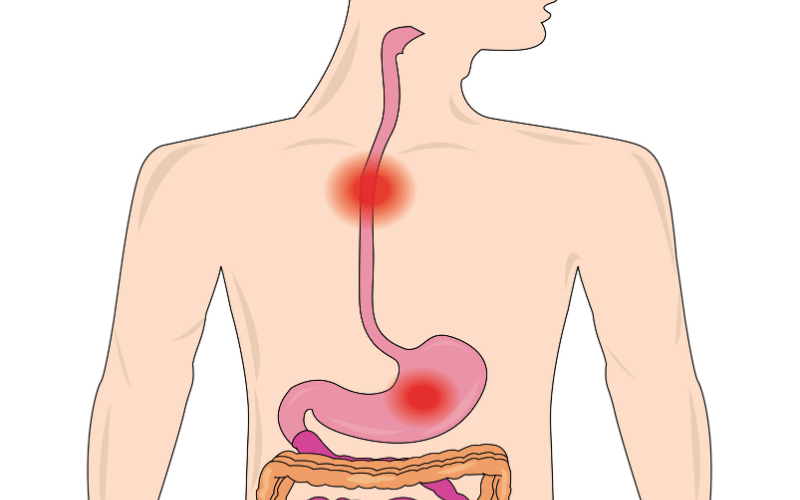
1. Difficulty Swallowing: The Peculiar Struggle in Esophageal Achalasia
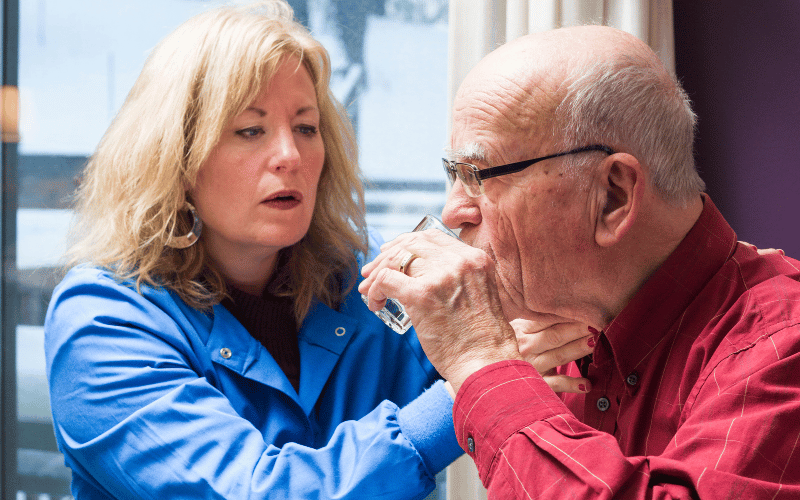
When it comes to esophageal achalasia, difficulty swallowing, or “dysphagia,” often leads the parade of symptoms. Let’s set the stage: you’re sitting down for a meal, fork in hand, and the first bite turns into an awkward, seemingly inexplicable battle with your own throat. You’re not choking; it’s more like your esophagus has lost its GPS and can’t figure out how to move the food down.
You might wonder what’s going on at a physiological level. Here’s the lowdown: the lower esophageal sphincter fails to relax. Imagine a security guard barring entrance at a VIP club; only this is at the entry of your stomach, and the guest list includes whatever you’re trying to eat. Even liquids can find themselves uninvited to this exclusive inner party.
Now, you’d think that forcing yourself to swallow harder might do the trick. Not quite. That’s akin to hitting a locked door with increasing frustration—it’s not budging without the right key. What’s interesting is how this symptom evolves over time; it starts off sporadic but gradually makes regular appearances, often extending its visit during every meal.
If you’re prone to self-diagnosis, you might mistake this symptom for just needing to chew your food more or perhaps slow down while eating. Make no mistake, dysphagia is neither a lifestyle flaw nor a momentary hiccup; it’s a signboard that’s hard to ignore, once you know what to look for.
And lest you think this is a symptom that’s easy to sweep under the rug, consider its impact on your social life. Imagine dodging dinner invites or awkwardly navigating through a meal at a restaurant, perpetually worried that swallowing the next bite could turn into a public spectacle. Yes, it’s that disruptive. (1)